Well, paint a placard and call me a scabber — it would seem I’ve made it into work today. Unfortunately, medical news doesn’t seem to respect the rules of industrial action. It’s a very demanding master.
I know i’ve let the team down… but can 3 research articles make up for it?
Yes? Wonderful 🙏
👋 Happy Friday. Here’s what we got:
🎭 Traitors: The Heart Attack Special
🫘 You Gotta Be Kiddn’-ney Me: Dialysis is Out?
☕ A Coffee a Day Keeps the Cardiologist Away?
🧠 QuickBits: Other Top Stories of The Week
If you want to read any previous editions of The Handover, you can on our website.
RESEARCH UPDATE
🎭 Traitors: The Heart Attack Special
There is an impostor among us… Do you know who it is?

Following a heart attack, secondary prevention is a must.
Aspirin. Clopidogrel. Atorvastatin. Ramipril. Spiranolactone. Bisoprolol.
Slap 'em’ all in a blister pack of pills and (hopefully) that’ll keep another infarct at bay 🙏
But you see, that’s the thing about group projects: there’s always one free-loader.
They doomscroll TikTok whilst everyone does the heavy lifting.
And one of these medications is looking suspiciously….ineffective 😑
Today, it’s Beta-Blockers being accused of being a bum 👀
Quick history lesson:
Back in the 80s, seminal studies like BHAT and ISIS-1(unfortunate name) had launched Beta-Blockers in ACS stardom. The cardiologist just loved that vasodilator.
But we’ve come a long way since then… Advances in cardiac diagnostics, reperfusion and revascularisation have got us questioning – are beta-blockers now a has-been like Britney Spears or Ronaldo?
What better way to figure it out than a meta-analysis?
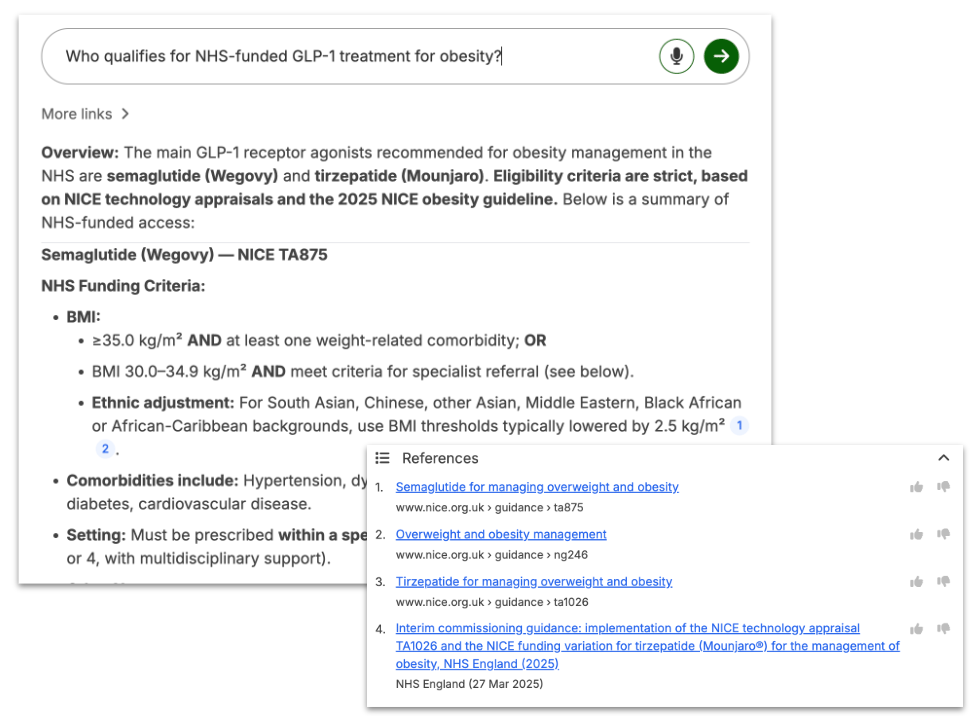
Published in NEJM this week, this investigation gathered 5 recent RCTs, including 17,801 patients.
They all asked the same question: In patients with a preserved ejection fraction(LVEF >= 50%), do beta-blockers actually help morbidity and mortality?
In these studies, participants were randomised to either:
A) Receive Beta-blockers
B) Skip them entirely
The primary endpoint was a composite of death from any cause, myocardial infarction, or heart failure.
What they found was this:
Beta-blockers did not significantly reduce the composite endpoint compared to no beta blocker therapy (8.1% vs 8.3%) (hazard ratio: 0.97; 95% CI, 0.87 to 1.07; P = 0.54).
A forest plot with a hazard ratio super close to 0. This means no clear benefit.
Even breaking down to its individual components barely made a dent. Comparing Beta-Blocker vs No-Blocker :
Death from any cause: 3.8% vs 3.6%, HR 1.04 (95% CI, 0.89 to 1.21)
Myocardial Infarction: 4.1% vs 4.5%, HR 0.89 (95% CI, 0.77 to 1.03)
Heart failure: 0.8% vs 1.0%, HR 0.87 (95% CI, 0.64 to 1.19)
These results were consistent across subgroups(based on sex, age and type of MI), and the beta-blocker given didn’t seem to have an effect either.
So it would seem that in patients with preserved ejection fraction, Beta-blockers seem to be as functionally useful as your appendix :/
But in the words of Uncle Ben: “With Great Research Comes Great Limitations” - or something along those lines…
All RCTs were open-label trials => increased bias.
The study population were European and Japanese => reduced generalisability
Differing primary endpoint definitions => increased heterogeneity.
Limitations aside, this study concludes with this:
In those with preserved ejection fraction, Beta-blockers remain on the post-MI team sheet. But their role is looking more like a squad rotator than a first-team starter.
POWERED BY MEDWISEAI
🤷 If Medwise Doesn’t Have the Answer…You’re Pretty F**ked
Anddddd there it is.
That one inevitable question.
The one you prayed wouldn’t surface in clinic 🫣
Or on the ward round.
Or in the seventh circle of hell, known as post-take.
You’re asked a clinical question you absolutely do not know. Not even vaguely. 🥀
Your senior: Missing In Action
The guidelines: 47 clicks deep on the intranet
GPT: Thinks Kawasaki is a Japanese motorbike :/
The pressure is on. And you’ve got nothing
If nothing else, remember these wise words:
If Medwise.ai can’t answer your clinical question… you’re f*cked.
Why?
Because Medwise.ai is like ChatGPT… if ChatGPT had been force-fed every NICE guideline, society consensus statement, and Royal College publication until it begged for mercy.
You type a question and bam:
Evidence-based answers
NICE-aligned. Instantly cited.
No more PDF trawling. No more second-guessing. No more panic-Googling behind a drug chart.
There’s a reason clinicians in 1,000+ NHS organisations already use it.
They stopped winging it. You can too.
So in 99% of clinical scenarios, Medwise.ai has got you covered
For the remaining 1%... I’m sorry.
Start looking dangerously competent on wards and use Medwise.ai today.
And use your NHS email address to get access completely free 👇
RESEARCH UPDATE
🫘 You Gotta Be Kiddn’-ney Me: Dialysis is Out?
So you’ve got an AKI. Bummer.
Not to worry! A multi-million pound, hospital-grade, expert scientist-engineered haemodialysis machine is here to take over for your two soggy pee beans.
Dialysis = pretty OP.
But also? A massive nuisance.
Imagine sitting through twelve full episodes of Andrew Tate’s podcast every week.
That’s how long a CKD patient spends hooked up to one of those bad boys.
Avoiding it where possible is a no-brainer.
But our poor little kidneys? It doesn’t take much to set them off.
Y’know, the little things…
A splash of sepsis
A minor cardiogenic shock
Or, say, our Jägerbombs post finals
… and they’re going on strike like [you fill in the blank 😉]
So: kidneys go kaput, dialysis swoops in to save the day.
Easy, right?
Not so fast, keen bean.
Published in JAMA this week, the LIBERATE-D trial asked this:
If we dial back the dialysis, could the kidney actually recover better??
The theory is this:
Frequent dialysis masks recovery signals and can injure kidneys via transient hypoperfusion and inflammatory activation from blood contacting the extracorporeal circuit. – in other words… You shouldn’t baby the kidneys into recovery. You gotta throw them back into action and work for themselves.
So what did they do?
Set up a multicentre RCT involving 220 adults with dialysis-requiring AKI
They were randomised to either a conservative strategy (dialysis only for specific triggers (e.g. K⁺ >6 mmol/L, severe acidosis, refractory pulmonary oedema) or conventional haemodialysis 3 times a week until recovery.
And what did they find?
In the conservative group 64% (70/109) achieved kidney recovery at discharge (alive and dialysis-free for ≥14 days) versus just 50% (55/109) in the conventional dialysis group.
That’s an absolute difference of 13.8% (95% CI; p=0.04)
Other wins for the conservative :
(Obvs) Fewer dialysis sessions (1.8 vs 3.1 per week)
More dialysis-free days (21 vs 5 out of 28)
Fewer hypotension events (69 vs 97)
Faster median time to recovery (2 vs 8.5 days)
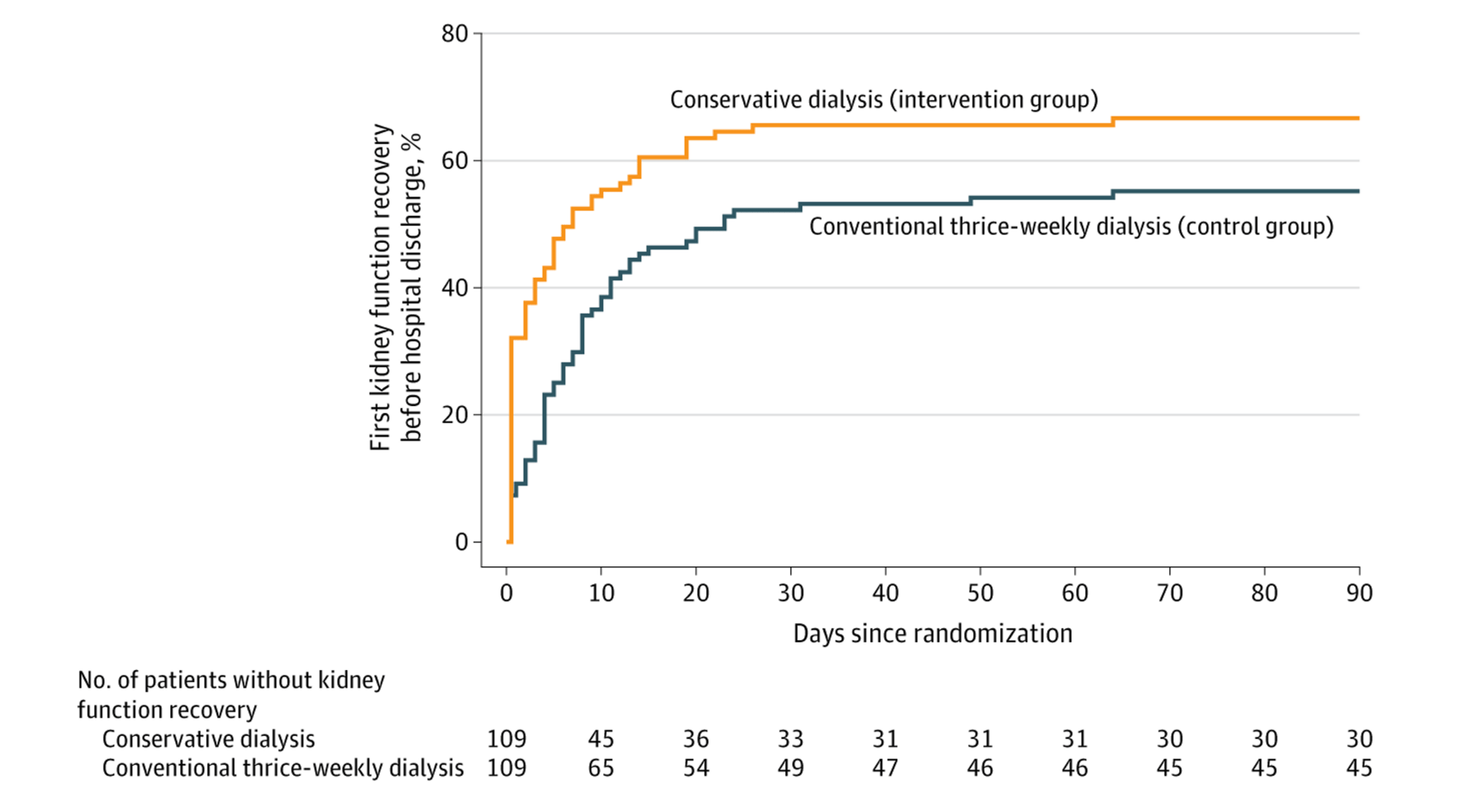
Kidney Stonks📈(time to first kidney function recovery before hospital discharge in the 2 groups)
But there are, as always, caveats:
Small study: Just 220 participants
Conservative dialysis relied on subjective clinician discretion for ~45% of sessions
Short follow-up period(15 days), so long-term renal implications remain a mystery
Participants were all stable adults with some residual kidney function
Unblinded - docs knew the group allocation, so bias in treatment decisions can’t be excluded
All in all: More studies are needed to confirm this conclusion.
So do your part as a research-committed medic:
Grab your mates, get absolutely smashed and don’t drink a single drop of water.
Time to see just how much cowabunga your little buddies can handle … in the name of science!*
* The Handover does not endorse self-induced AKIs, binge drinking or any attempt to provoke organ injury for the sake of curiosity. There are easier ways to get portfolio points, I promise.
RESEARCH UPDATE
☕ A Coffee a Day Keeps the Cardiologist Away?
Cardiologists love to sing the gospel.
To their patients. To clueless non-specialists.
To whisper it down the phone while rejecting your referral at 3 a.m.
“We’re not an ECG interpretation service”
“It’s not cardiac”
“Are you sure they don’t smoke. With these coronaries?”
“No. Obviously, they shouldn’t drink coffee with AF”
Ok, we made that last one up. But here’s a question:
If you’ve got a history of AF, what do you think loads of coffee does?
Here’s what you might have been taught. Caffeine = AF recurrence risk factor.
Zero to Finals even says it, so it’s basically scripture.
The physiology checks out, too:
Adenosine is our crash-trolley bestie. But it’s also endogenous. It slows AV node conduction and chills everything out. Caffeine blocks its receptors(a real enemy of progress).
Plus, caffeine triggers catecholamine release → beta-adrenergic stimulation → faster heart rate, higher contractility, lower refractory periods…
And that transient caffeine BP rise? More atrial stretch. Stretchy atria = spicy atria.
So? Case closed: Caffeine No Good.
But observational studies couldn’t make up their mind…
A 2022 meta-analysis even concluded caffeine might reduce AF risk.
What was missing was trial evidence. Until now…hold my mug.
Enter the DECAF trial - Does Eliminating Coffee Avoid Fibrillation? Yes, that’s the actual study name.
This multicentre RCT, published this week in JAMA, randomised 200 regular coffee drinkers who’d just been successfully cardioverted after an episode of AF (or flutter with a history of AF).
Two arms:
Coffee group: Drank their regular caffeine intake (minimum one cup/day).
No-coffee group: Abstained from coffee and all other caffeine. Poor souls.
The result?
Those who kept sipping their morning brew had a lower recurrence of AF.
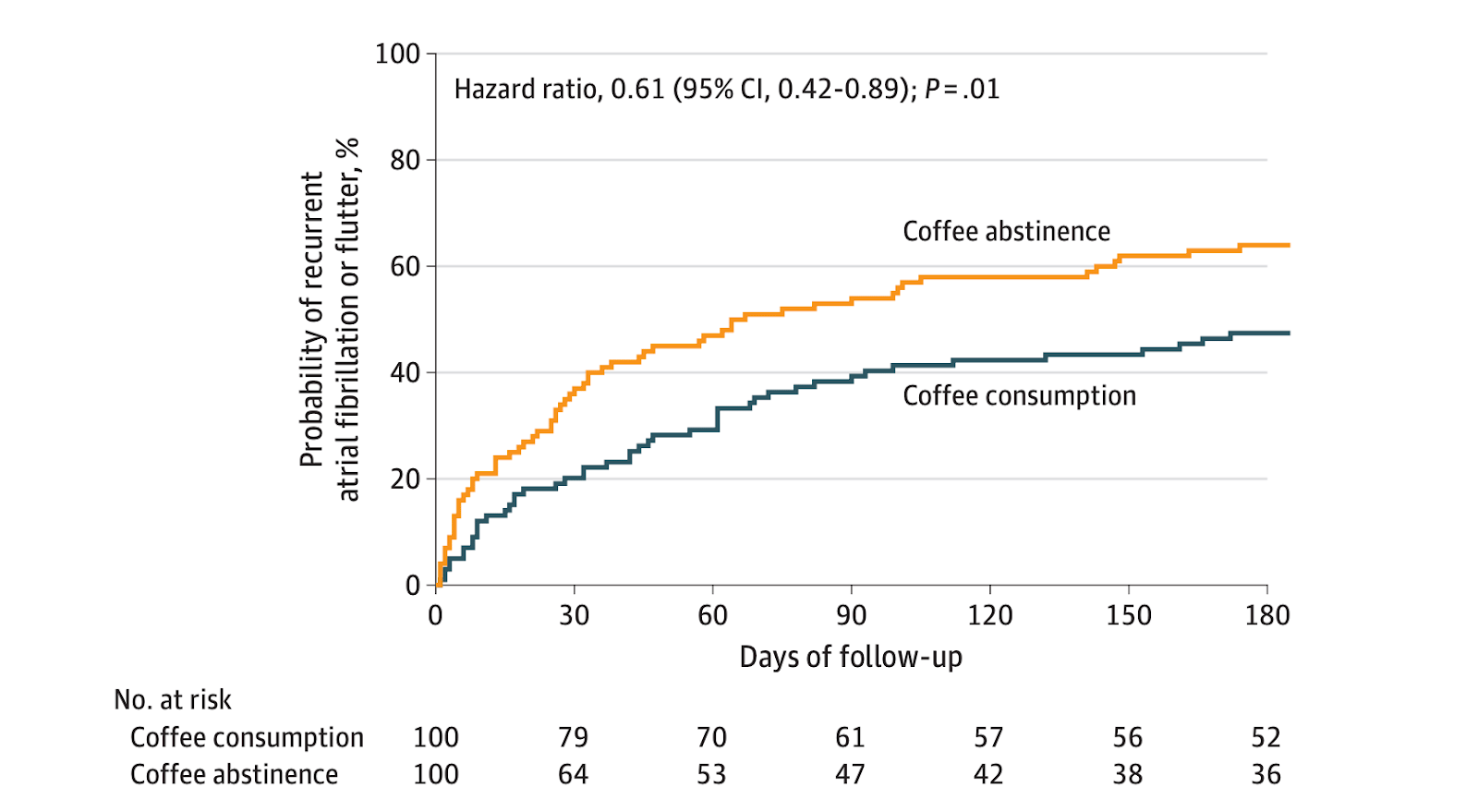
After 6 months:
47% (47 of 100) AF or flutter recurrence in the coffee group.
64% (64 of 100) recurrence in the no-coffee group.
A 37% hazard reduction for AF recurrence if you kept drinking the beans.
And no extra strokes, heart failure, or admissions.
So coffee is protective? We’ll drink to that ☕
But hold on. Spill the (limitation) beans
It was non-blinded: Everyone knew exactly who was caffeinated vs who was cranky.
The AF detection was messy: ECGs, Apple Watches, implantables. ‘Recurrence’ was defined as the clinically irrelevant 30 seconds of AF, which isn’t exactly life-altering.
Only one cup/day required: What about the triple-shotters?
This doesn’t prove caffeine is protective. It just suggests that continued moderate intake might be better than an abrupt caffeine break-up.
The final sip?
When your AF patient asks: “Should I stop drinking coffee?” You can say going cold turkey probably isn’t going to do their atria any favours.
And next time cardiology goes off at you at 3 am
Smile, don’t stress.
Sip your coffee confidently.
Your rhythm could be more stable than theirs.
QUICKBITS: OTHER NEWS YOU SHOULD KNOW
We’ve seen some many injectable brainchips by now. But this one’s a lil different. Forget the invasive and tedious craniotomy. A simple IV injection lets these chips travel through the blood, past the blood-brain barrier(much to the jealousy of dopamine, ifykyk) and directly into the brain. It can then be used to treat Alzheimer’s, Multiple Sclerosis and tumours.
The Desolate and Decrepit GPland
According to a poll conducted by the RCGP, nearly a 1/3 of GPs are unlikely to be working in general practice in 5 years… yikes. What’s the reason for this mass GP exodus? Stress, of course! Interesting stats include: 44% think of alternative careers, 39% plan to retire and 28% report they feel so stressed, it’s difficult to cope. It’s okay though. I’m sure adding GP Online to 100% helped this stress burden. Great shout from Wes…
Trump won’t be pleased with this. We can now do surgeries in America without a Visa! A world first was completed this last week, with a surgeon in Dundee conducting a thrombectomy for a patient in Florida. Completely remotely, via a robot. This can be a complete game-changer for people in remote areas without access to specialist stroke facilities. H1-B Visa who?
Last week, we reported that OpenAI would do a better job at referring patient enquiries to real doctors. However, hasn’t stopped AI from being an increasing force in self-diagnosis. An estimated 9% of men and 7% of women in England use AI chatbots for health advice and information. Another 21% of women and 18% of men are using TikTok, Insta and YouTube for health advice. When you have people like Dr Berg(not an MD, actually a chiropractor) with 14 million followers dishing out health advice, at least we know our patients are in safe hands.
This Handover is Over 🫡
If you liked it, tell your mates.
If you hated it, tell your enemies.
Please vote in the poll below(even if you’ve voted before!)
What did you think about todays handover?
What you don’t know is that in our writers group chat, we share, smile and laugh at all the comments you make.
The best ones will feature on our(recently updated) website - so please comment after you vote 😘 + share the handover with a friend and forward this email on
Wait!
Before you go(if you haven’t voted already), please let us know your role in the poll below - It means the world when you do 🫶
Fun Fact: Some deaf people with tourettes syndrome involuntarily sign curse words with their hands.
If you want to get in contact with The Handover, email us at [email protected]
The Handover is intended for healthcare professionals and does not constitute medical advice.