Happy Sunday 👋
Judgement Day is upon us. Medical Ragnarok has arrived. The Leng Review has been released.
Yes. The one you’ve all been waiting for. After months of frothing controversy, leaks and unhinged r/doctorsUK threads (admit it, we’re dramatic), Professor Gillian Leng has dropped her independent review into PA’s and AA’s. 134 pages of deep dives into the roles, the evidence, and what it all means for the NHS.
And I’ve got to say… after all that build-up, the conclusions are really… lukewarm?
Yeah, the review is pretty on-the-fence. The overall conclusion is PAs and AAs should neither be abolished outright nor left to continue unchanged. It validates doctors' feelings, whilst at the same praising the PA's value to the MDT. How delightfully diplomatic…
But still, it drops 18 recommendations based on the available evidence.
We dropped the high level summary two weeks ago, but you were hungry for more. Alright Oliver. Unlike Mr Bumble, I’ll gladly oblige.
Last time, we covered key points such as PA safety, supervision rules, and role changes. To get you up to speed, here’s the link to last week's article.
Today, we’ll expand upon the previous issue. We promised more recommendations, more detail and more novel insights. On those points, we will deliver.
Ready? Let's do it!
IN PARTNERSHIP WITH ACCURX
Say it with me: I AM NOT A WARD MONKEY! 🐵
You’ve done a ward round, five clerkings, and an MDT that ran 47 minutes over. You deserve a coffee break… and a Thai massage.
Instead, you get the gift of documentation.
...What was the first patient's name again?
No. No more.
You. Aren’t. A ward monkey.
You’re a clinician. A great one at that!
Start acting like it and leave the monkey work to Accurx Scribe.
It helps you complete documentation in seconds. Tap once. Speak as you normally would.
It’ll capture your conversation, turning it into structured notes and auto-generated discharge summaries, clinic letters and handovers.
Surely you can’t actually use this? You can! It’s a registered MHRA Class I medical device– meaning it’s approved to use in the clinical setting and inline with NHS guidance.
Now available in the Accurx App, it’s your ears across:
Ward rounds – dictate in real time, cut down write-ups.
A&E – record as you go, in a high pressure environment.
MDTs – summarise decisions that aren’t just scribbled on the back of the patent list.
Clinics – finish notes before the next patient sits down.
That’s clear documentation. Done fast. Done right.
Get back to the important tasks. Leave on time. Used by 120,000 healthcare professionals already. Check out Accurx App today 👇
Still not sold? Check out the demo video below
SUNDAY DEEP DIVE
The Leng Review: Casually Explained
Teamwork makes the dream work.
We all know the MDT is the powerhouse of the healthcare system. PAs/AAs were partially introduced to oil the engine and enhance team-based care. To their credit, in accordance with the findings of the review, they have done just that.
Findings: According to the review, testimonials from senior clinicians working directly with PAs sang their praises. PAs in hospitals were valued for:
Continuity of care (due to staying longer in departments than rotating junior docs).
High standards of commitment.
Excellent communication skills.
Performing routine procedures (lumbar puncture, IV lines), allowing doctors to do other things.
Moreover, in some instances, the really good PAs allowed for service expansion. That's a dedicated procedure service run by PAs, which isn’t feasible with only rotating doctors. Qualitatively speaking, the PAs can be a great helping hand. But between those lines, lies the first problem… There is a large dissonance between what PAs think they’re capable of, and what doctors think they’re able to do.
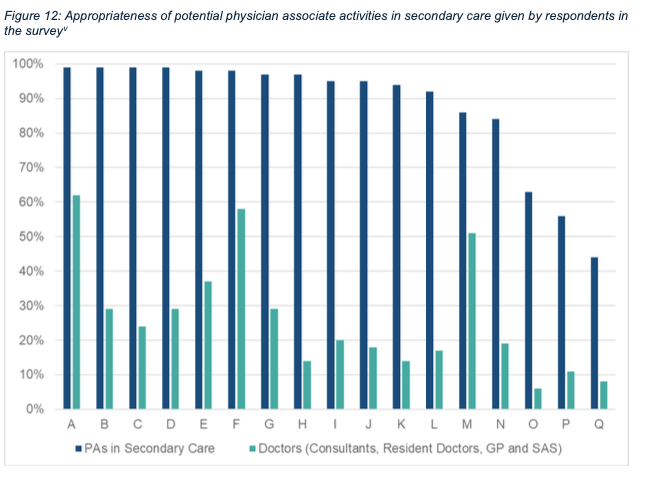
The graph above shows how PAs rated how well they thought they could handle 17 different secondary care tasks.
They were feelin’ themselves. For 12 of those 17, they gave themselves a solid 90%+ on the “I should be doing this” scale. They’re 90% confident about performing physical exams, clinical assessments, reviewing tests, writing management plans, even diagnosing illnesses and more.
The doctors’ approval rating wasn’t quite the same… only 3 of those 17 tasks even scraped above a 40% approval rating from doctors. The three that doctors were semi-okay with PAs doing were providing health promotion and prevention advice (62%), supporting research and audits (58%) and delivering immunisation (51%).
This disconnect highlights the massive mismatch in expectations. Where role boundaries start getting fuzzy, the dream team starts to underperform like the England men's football squad.
Junior doctors (JDs) felt sidelined when PAs got those juicy, but scarce, learning opportunities.
JDs felt dumped on when they were suddenly made to supervise a PA, without the training (or time) to do so
Consultants were also weary about supervising eager PAs. Appreciate the enthusiasm, but it's on their head if it goes wrong.
This friction created a workplace environment more toxic than Britney Spears in 2003. According to the review, the problem was baked in from day one: teams were handed new professionals without redesigning the system around them. PAs were dropped in like plug-and-play junior doctors… except they’re not. So the system got the worst of both worlds: underused PAs and overworked, annoyed doctors.
Recommendations - based on these findings the relevant recommendations were:
Recommendation 6: “[the PA’s] role should form part of a clear team structure, led by a senior clinician, where all are aware of their roles, responsibilities and accountability” — practically speaking, this means PAs are formally assigned to specific firms or consultant-led units rather than floating ambiguously.
Recommendation 17: “DHSC (Dept of Health and Social Justice) should establish a time-limited working group to set out multidisciplinary models of working in different settings” — this recommendation acknowledges that ad hoc evolution of roles has led to this mess. Official guidance in all settings should be put in place.
Recommendation 16: “Doctors should receive training in line management and leadership and should be allocated additional time to ensure that they can fulfil their supervisory roles, and to ensure effective running of the health service” — basically, the goal is to leverage the complementarity of the roles: PAs focus on the routine/protocol aspects of care. Leave the complex stuff for the doctors and train them so they know how to do so.
So this is as good as it gets?
Much of the controversy surrounding PAs (especially following the recent strikes) is that juicy 50k-a-year starting salary. Is that wage justified? Idk, I'm not an economist. But… it does overshadow the foundation year's salary by around 30%. And we’re supposed to supervise them… I don’t have to be a mathematician to see that things are not adding up 🤔
This is no fault of the PAs, of course. You gotta go where the getting is good. If money is the motivation, their financial decision-making far exceeds us medics.
But the problem with that starting salary is that it's also their ending salary. It actually doesn’t get any better than that. It’s not just their wages that are stagnant. It’s the whole career.
Findings: There is currently no formalised training programme or career progression pathway for PAs or AAs post qualification. Many undergo additional training and accreditation to enhance their knowledge and skills, but there isn’t actually a means of going up the ladder. There is no ladder. Just a single step.
The review states: Without progression, PAs/AAs remain generalists. Now, if you put these generalist PAs into speciality locations, this could potentially risk patient safety or hinder service delivery.
Mental health’s a good example. PAs there often handle physical healthcare, but under supervision from mental health staff, not physical health teams. The problem is, these patients are complex. They’re on unusual meds, juggling multiple conditions, and need more than just basic checks.
In any other setting, they wouldn’t be handed to a newly qualified PA. But here? It happens. And that’s a system issue, not a staff one.
Recommendations - several measures address training and career progression concerns:
Recommendation 2: “Physician assistants should have the opportunity for ongoing training and development in the context of a formal certification and credentialing programme. This should include the ability to take on added responsibilities that are commensurate with that training, including the potential to prescribe and order non-ionising radiation.”
Recommendation 3: “Physician assistants should have the opportunity to become an ‘advanced’ physician assistant, which should be one Agenda for Change band higher and developed in line with national job profiles.”
Recommendation 5: “Newly qualified physician assistants should gain at least 2 years’ experience in secondary care prior to taking a role in primary care or a mental health trust.”
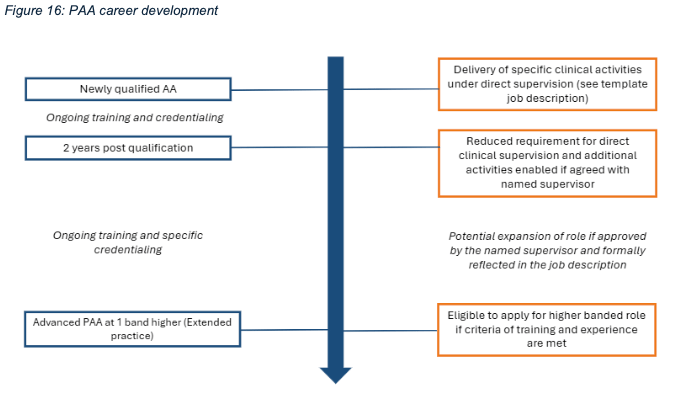
The above points increase the scope and pay of PAs, rewarding the enthusiasm shown by PAs in Leng's audit. These points have also been a source of contention amongst doctors. To many it seems like another step towards scope creep; it also shows that the government has money to spend, but is still reluctant to address pay restorations. Recommendation 5 was put in place to ensure PAs get broad clinical exposure before they operate in environments with more free reign (like GP clinics).
What else is there to know?
1. Ignorance is not bliss
The review uncovers a systemic blind spot: current NHS incident reporting doesn’t capture the role or profession of staff involved in safety events. Current incident reports don’t record who was actually involved!
So if certain errors are cropping up more often with, say, newer staff or specific roles, we wouldn’t know. Right now, everything’s blended together in the name of avoiding blame. Which is good for morale, but bad for spotting patterns.
Insight: We gotta start tracking incidents by staff group. And it’s about the blame-game. It’s about smarter prevention. If data shows, for example, that PAs are more likely to run into med errors, you can adjust training or support before things go wrong.
Recommendation 18: “Safety systems should routinely collect information on staff group to facilitate monitoring and interrogation at a national level, against agreed patient safety standards, to determine any system-level issues in multidisciplinary team-working.”
2. Oh captain my captain …Where’s my captain?
A less obvious reason things stalled was that medical leadership in the NHS is split up and disconnected. The report points out that in earlier eras, a single Chief Medical Officer had broad authority to steer the ship.
Now, leadership is dispersed among various national and local medical directors. All these CCGs, ICBs are really confusing. It's all split across a bunch of national and local directors. This means there’s no clear voice, no unified strategy and no one really steering the integration of PAs and AAs.
Insight: Now bundle this with doctors being handed management roles they weren’t trained for. You get this awful governance vacuum: no clear direction from the top, and not enough support from the bottom.
The review doesn’t call for a full-blown leadership overhaul (we’re still reeling from the death of NHS England). But the bottom line is: train your doctors, strengthen structures, and give teams proper oversight. Simple 👍
Recommendation 14: “A permanent faculty should be established to provide professional leadership and set postgraduate standards for physician assistants in anaesthesia, under the auspices of the Royal College of Anaesthetists.”
3. How can I trust you now? 😪
A final underappreciated risk of the PA/AA rollout was its impact on patient confidence.
The review’s pretty blunt about this. Public trust depends on being upfront about who is treating you. And when a patient finds out halfway through that the person they thought was a doctor... isn’t? It’s a little concerning. It might not spark full-blown outrage, but it chips away at trust. They might second-guess the care, or hold back on stuff they’d normally share.
Insight: Ensuring that patients understand the roles and titles of those treating them isn’t just a courtesy — it’s fundamental to patient-centered care.
Recommendation 1: “The role of physician associate should be renamed as ‘physician assistant’, positioning the role as a supportive, complementary member of the medical team.”
All in all, the review covers a lot of ground, but one thing’s clear: PAs and AAs aren’t going anywhere. So rather than dragging out the “us vs them” turf war, it’s probably time to start thinking like a team. If you can’t beat em’, join em’… or rather let em’ join us.
With the right structure, leadership, and communication, the recommendations actually lay out a semi-decent path forward. Not perfect, but a start. A way for doctors and PAs to stop coexisting awkwardly and start actually working like a team.
Nice. You made it all the way through.
Thanks for reading. If you found this useful, please forward this email to one friend (or two if you’re feeling super generous!)
And I hope you enjoyed today’s deep dive. Let me know what you thought in the poll below. Every vote helps!
What did you think about todays handover?
Thank you again to Yuna Chow for editing todays edition.
See you next Friday, for the regularly scheduled programme 🫡
Last chance. This is your last chance to tell me about yourself. If you haven’t voted already, please do in the pole below 👇
That was a empty threat. I’m totally asking again next week 🙈. Thanks anyway


