Take a deep breath in…
Ahhhhh. Smell that?
Y’know, nothing hits quite like the sweet scent of fresh medical literature.
Well…technically, that’s a lie.
But if you think you get that special mix of disinfectant, blood and burnout anywhere else… let me know, it’s probably less carcinogenic.
👋 Happy Friday. Here’s what we got:
🤯 Breaking News: Binary Guidelines Too Simplistic
⚖ You vs The Tribunal: The DMARD Dilemma
🧠 QuickBits: Other Top Stories of The Week
If you want to read any previous editions of The Handover, you can on our website.
RESEARCH UPDATE
🤯 Breaking News: Binary Guidelines Too Simplistic
Time to quiz you little nerds … who can tell me how long we treat a provoked VTE for?…..…Anyone??
To the trained Passmed monkeys who blurted “3 months!”, well done.
Have a cookie 🍪
But just pause that Pavlovian hand-raise for a sec.
Why three months? Why not two? Four?
The HI-PRO trial, which just dropped in the New England Journal of Medicine, asks the annoying but important question: what if VTEs aren’t just a simple binary?
To investigate, they recruited 600 adults who’d had a provoked VTE (surgery, trauma, immobility) but also carried at least one enduring risk factor. Think obesity, chronic disease, all that fun stuff.
After 3 standard months of anticoagulation, participants were randomised to either apixaban 2.5 mg TDS OR placebo for 12 months.
What did they find?
Symptomatic recurrent VTE in the apixaban group: 1.3%
Symptomatic recurrent VTE in placebo group: 10.0%.
That’s a hazard ratio of 0.13 (95% CI, 0.04 to 0.36, P < 0.001)- An ~87% relative risk reduction.
Translation for those of us still struggling with stats (me): treat twelve similar post-provoked-clot patients with apixaban for a year, and you’ll prevent one symptomatic VTE that would’ve otherwise happened.
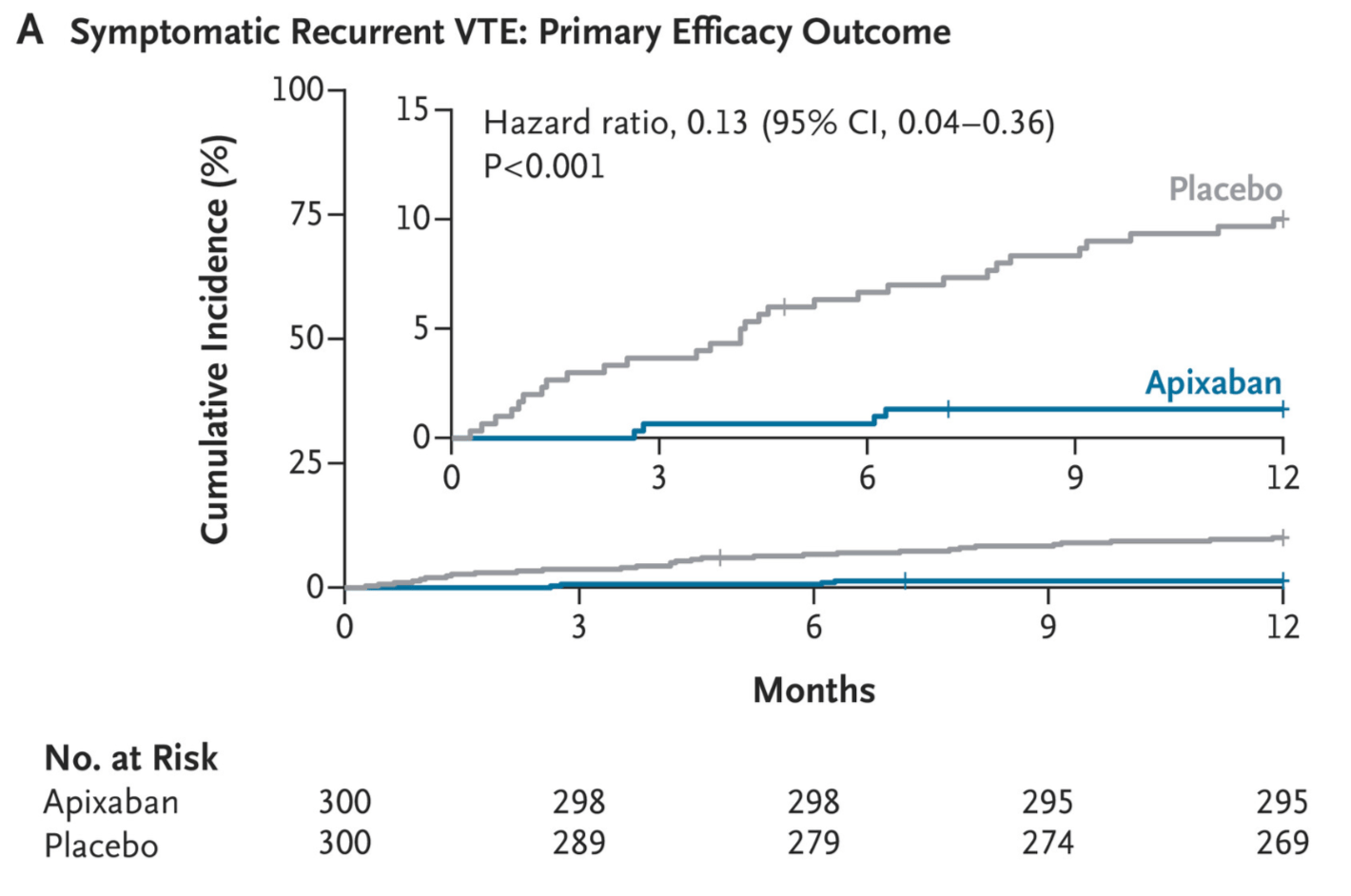
But what about bleeding?
Major bleeding was rare with only one event in the apixaban team (a subdural after a horse fall; no hospital stay, no death, no big deal)
Lesson learnt: apixaban prevents clots, not the consequences of foaling around 🐴
Non-major bleeding, however, was more common with apixaban: 4.8% vs 1.7% (95% CI, 0.96 to 7.43, P = 0.06)
So, although big boy bleeds were almost nil in this cohort, non-major bleeds were more common and therefore worth factoring into clinical decisions.
(Limitations to bear in mind: all participants in HI-PRO were recruited from the same hospital, and cancer-associated VTE and severe thrombophilia weren’t taken into account.)
Why does this matter?
Because it suggests the categorisation of VTE isn’t so black and white. Provoked/unprovoked clots are neat for SBAs but not so much for real people. Especially patients whose clots were technically provoked but with a background risk.
In this trial, the unlucky placebo group had a 10% recurrence rate at 12 months. So it’s giving less “safe to stop”, more #apixaban4lyfe.
So the VTE TDLR;
UKLMA? 3 months.
Real life? Not so simple.
Hotel? Trivago.
POWERED BY BMJ ONEXAM
Forget Everything You Know About The BMJ
You’ve trusted them.
Cited them.
Built your essays, your audits and your reputation on their words.
But with this journal, there is more to what meets the abstract…
Because within The BMJ Group, a specialised internal team of experts has been working quietly behind the scenes…
Channelling years of academic expertise into a covert project designed to help medical trainees do one thing: Pass. Everything.
Pre-Clinical Exams. PSA. UKMLA. MSRA. MRCGP. MRCP. NCE CBT. SCE.
Cradle to Grave. They covered it all.
It’s called BMJ OnExam.
And no. It's not just another generic question bank.
Every single item is clinically reviewed, peer-checked.
Then patterned to the real exam format.
That’s right, question stems as short as Kevin Hart.
Get a feel for it. No shocks and no surprises on test day.
High Impact Question Only.
Plus:
BMJ OnExam App: The most comprehensive exam mobile app out. Finding time between work is hard enough. Available offline, keeping you on point and on track ✅
Mock Tests: Like the real thing, but without the existential dread (mostly).
Group Learning: Learning doesn’t have to be lonely. OnExam ensures that.

I’m not asking for blind faith.
We’re about evidence-based practice here.
OnExam helped over 100,000 HCPs this year alone.
See for yourself. Dip a toe in. Test-drive OnExam for free.
Plus, we managed to sneak in a cheeky 40% discount for you too.
Just use HANDOVER40 using the link below 👇
RESEARCH UPDATE
⚖ You vs The Tribunal: The DMARD Dilemma
Perhaps no condition better embodies the image of malevolence than arthritis.
It’s chronic…
It’s cruel…
And it’s got more variants than a corner shop vape rack.
Thankfully, we have modern medicine. Blessed be the biologics.
TNF inhibitors, JAK inhibitors, plus trusty ol’ methotrexate and steroids
These immunomodulatory agents(IA) sing a sweet lullaby to the immune system, soothing it into silence.
Which is all well and dandy… until there’s actually an infection to fight.
So you’ve got this patient on DMARDs and a spiking fever…
What’s your next move?
Pause the meds and risk a serious flare-up.
Or continue them, and risk an infection that makes the flu look like foreplay?
Let’s consult NICE guidance… Nothing
What about research? …There is none😕.
No one has properly studied whether continuing or stopping therapy actually changes outcomes in this massive group of patients.
So all we can do is risk it with our clinical judgement.
But to my knowledge, vibe-based medicine has yet to win a tribunal case…
So… what the hell do we do?
Thankfully, the Dutch delivered.
In this multicenter, open-label RCT, published in the Journal of Clinical Infectious Diseases, researchers aimed to investigate and directly compare the two strategies.
Should we continue IA therapy during infection or temporarily stop it?
Conducted across the Netherlands, they recruited 1,142 patients. The requirements were:
To have an Inflammatory rheumatic disease(IRD)
On an immunomodulator treatment
Without an active infection at baseline.
Researchers then waited (as patiently as one can with 1,000+ immunosuppressed patients) until each developed their first clinically relevant infection(CTCAE grade ≥ 2). 474 patients met this criterion.
These patients were randomised 1:1 to either the continuation or interruption groups.
The primary outcome was to measure the proportion of those patients who developed a serious infection(requiring hospitalisation or IV treatment) in each respective group.
The results came in, and this is what they found:
Serious Infection Rates: In the pause group, serious infection occurred in 5.15%(12 of 233) of patients, whilst in the continue group, infections occurred in 3.73%(9 of 241) of patients. Pretty surprising.
Risk Difference: The adjusted risk difference of 1.71%(95% CI: -1.99 to 5.39) in favour of the continuation group was confirmed as statistically insignificant.
Other Outcomes: These patients were twinning pretty much in every other regard. Similar duration of infection, similar disease activity after infection and similar causes of infection(mostly COVID-19 ).
So…no meaningful difference between groups.
And paradoxically, continuing meds was slightly safer in absolute terms.
That said, we’re talking about a 3-patient difference. Plus, it was an open-label trial– some folk didn’t stick to their group, ultimately blurring precision.
Still, the takeaway is clear:
In patients with moderate disease, there’s now a solid argument for continuing treatment through infection.
Of course, it’s not gospel. Clinical context still matters.
But now you’ve got more than just vibes to back you up.
And that… might just win your next tribunal case.
QUICKBITS: OTHER NEWS YOU SHOULD KNOW
GPs Back in War Mode – The BMA has re-entered formal dispute with the government over new GP rules forcing unlimited online consultations from 8 am–6:30 pm…with no extra staff, and no way to tell urgent from non-urgent cases. Wes Streeting actually compared booking a GP appointment to getting a haircut appointment… a haircut. GPs are rightly furious, but the general public has never been more pleased. The Department for Health are dropping 10-year-old Drake memes celebrating the reform. Pending implosion? Imminent.
NHS and First Cousin Marriages 👍 👎 - NHS England deleted a blog on first cousin marriage after backlash over claims it had “potential benefits.” Critics called it disgraceful, experts called it factual, and Twitter had a field day. The piece was meant to inform clinicians, not back cousin weddings. But with a ban bill heading to Parliament, the NHS is now very much saying: We don’t want any part of this.
22 Banned Doctors Working In The NHS - In this Times exposé, 22 doctors who have been banned in their home countries have been found working freely here, in the UK. Kinda like Medical Mike Ross from Suits, except this isn’t fictional. Wes(naturally) said this is a massive disgrace. We are losing training places to banned doctors, I can’t make ts up😂.
Corsodyl Stocks To The Moon Boys 🚀 - A massive study just linked gum disease bacteria like P. gingivalis, a known cause of gingivitis, to a tripled risk of pancreatic cancer. Researchers analysed spit from 120,000 people and found a mix of mouth bugs (including Candida) that could predict cancer years in advance. Now, I don’t know much about meme stocks, but I’m going long on Corsodyl (this is not financial advice)
Handover Over 🫡
If you liked it, tell your mates.
If you hated it, tell your enemies.
Please vote and give your opinion in the poll below(even if you’ve voted before!)
What did you think about todays handover?
The FIGs Scrubs Challenge may be over, but if you love The Handover, please continue sharing the word.
We’re sooo close to 10,000 Handovians in the Community, our end-of-year goal. We could do it this week, with just a little push.
So please share The Handover using your personalised referral link below. Or, if its easier, forward this email to one friend.
N.B. Referral gotta be nhs.net, doctors.net or a university email address. Referral requires double opt-in verification, so tell your mates to check their email after they sign up!
Before you depart(if you haven’t voted already), please let us know your role in the poll below - It means the world when you do 🫶
Fun Fact: JAK inhibitors get their name from Janus kinases, after the Roman god Janus, the two-faced god of beginnings and transitions. Just like Janus, these enzymes have a “dual head” structure, which inspired the name.
If you want to get in contact with The Handover, email us at [email protected]

