September: The month of bipolar weather. One day it’s torrential rain, the next sweltering heat— then both like the final scene for a 2010’s rom-com. Pack the parka, or pack the sunshades? The inconsistency will drive you insane.
At the very least, you can depend on us for your weekly fix of medical news.
👋 Happy Friday. Here’s what we got:
👴 ❤ A Geriatric Love Story
💊 🤔 New Antibody, Who Dis?
🧠 🧠 QuickBits: Other Top Stories of The Week
If you want to read any previous editions of The Handover, you can on our website.
RESEARCH UPDATE
🧓 ❤ A Geriatrics Love Story
It’s 8pm on a Friday.
You’re on geriatrics
Your shift should have ended an hour ago.
But unfortunately, you're the sucker too honest to lie about your imaginary kids' dance recital 💔.

The NHS and ward manager salute your integrity. Your co-workers are cosy, watching Love is Blind right now
Now it’s just you and a ward of elderly folk, with different elderly problems.
Let’s do a quick roll-call:
Dani has dementia. Fawn keeps falling. Ilona is incontinent.
Norman has all three. He’s wet, wobbly and wacky.
Textbook normal-pressure hydrocephalus.
No problem. Just have a chat with neurosurgery, put a shunt in and voila – Norman’s normal again...Right?
Well, no. Of course not.
The problem is that shunting is kinda like the “keto diet” of neurosurgery: small evidence base, strong placebo effects and questionable long-term gains.
The literature’s been begging for more studies to be done to see if shunting is actually worth the hassle.
Their prayers were answered.
Published in the New England Journal of Medicine, this trial aimed to figure out if shunt surgery actually improves symptoms in patients with idiopathic normal pressure hydrocephalus(iNPH).
This multicentre RCT recruited 99 participants. They were included if they had iNPH, if they could walk 10 meters unaided and could walk a speed of 1.0m/sec or more.
They coin-flipped patients into one of two groups:
Open shunt group (49 patients): The shunt valve is set to an opening pressure of 110mm of water.
Placebo group (50 participants): The shunt valve was set to an opening pressure of over 400mm of water. A pressure so high nothing was getting drained.
3 months after the surgery, all three cardinal symptoms were measured: Gait velocity was the primary outcome measure. Cognition and continence were secondary, measured using MoCA and the Overactive Bladder Questionnaire respectively.
TLDR: Shunting works… partially.
Wobbly: In the treatment group gait velocity improved by 0.23 m/sec. This contrasts the placebo which did nish (0.03 m/sec improvement). This net shunting a sweet and significant 0.21 m/sec improvement over placebo (95% CI, 0.12–0.31; P=0.001).
Wet: There was no significant difference in the Overactive Bladder Questionnaire.
Wacky: There was no significant difference in the MoCA score either.
So whilst Norman may be steadier on his feet, he’ll still soak the bed and confuse the consultant for his late wife, Margaret(Mr Gravenberch is a bit androgenous looking tbf).
Perhaps if the trial didn’t exclude those who couldn’t 10 meters alone, those on long-term anticoagulants(which is most over 70’s) and recorded over a longer time horizon the findings might have been different.
Regardless, when iNPH is involved, shunt ahead…
It’s legit the only management we have for this condition anyway.
POWERED BY MEDWISEAI
🙏 Don’t Be A Laggard
After years of study, researchers out of the prestigous University of Handovia have finally adapted the Technology Adoption Cycle to the healthcare setting.
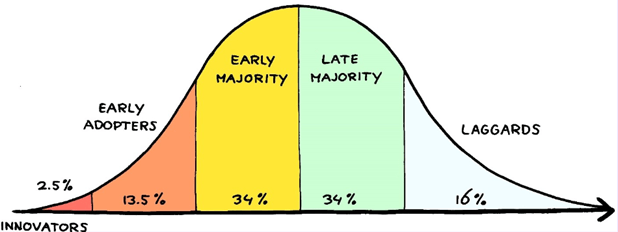
Stage 1 is Innovators That Weird-Ass Reg in Your MDT
Jamie’s gone off again.
Last year it was NFTs. Then memecoins.
Now it’s this “GPT for doctors” thing.
You roll your eyes.
Stage 2: Early Adopter Did You Hear He’s Really Clever Now?
Suddenly Jamie’s… useful.
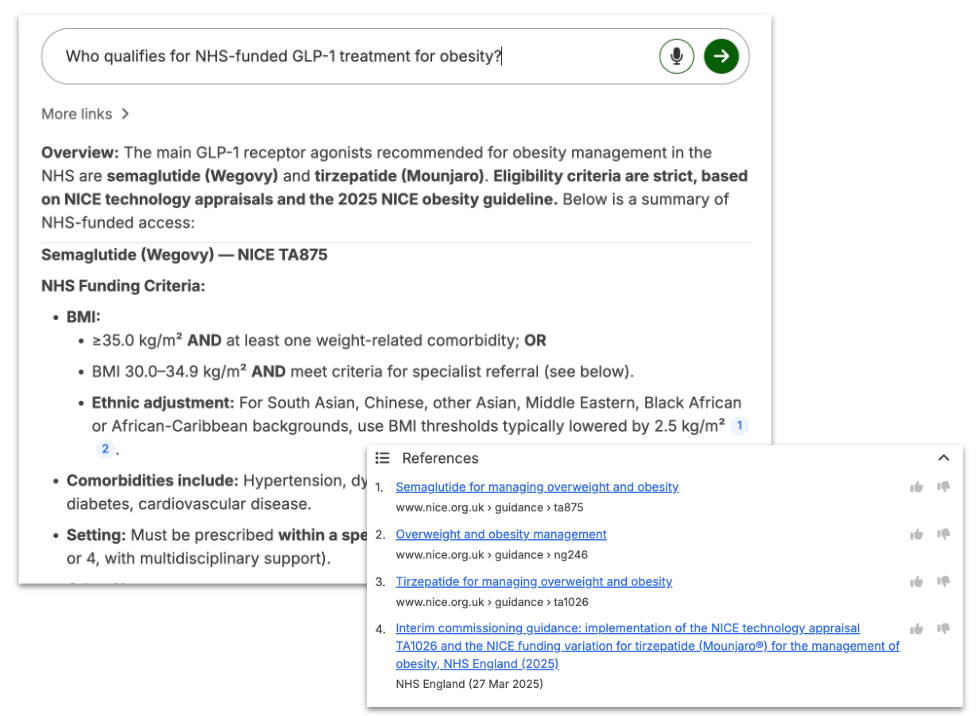
He’s quoting NICE guidelines published last week and referencing trust guidelines like their trending on Twitter. The consultant loves him. The whole team loves him.
What the hell happened???
Stage 3-4: How Bad Could it Be?
You crack.
What was that site again?
It’s called Medwise.ai
It’s like ChatGPT but force-fed every NICE guideline, society consensus statement, and Royal College publication until it begged for mercy.
You type in a question and bam.
Evidence-based answers.
NICE-aligned. Instantly cited.
No more PDF trawling. No more second-guessing. No more paging Jamie.
And apparently, it’s already used by over 1,000 NHS organisations.
So avoid becoming a Stage 5 Laggard and try Medwise.ai today
And if you sign up with your NHS email, you’ll get access completely free.
Check it out with the link below 👇 :
RESEARCH UPDATE
💊📲 New Antibody, Who Dis?
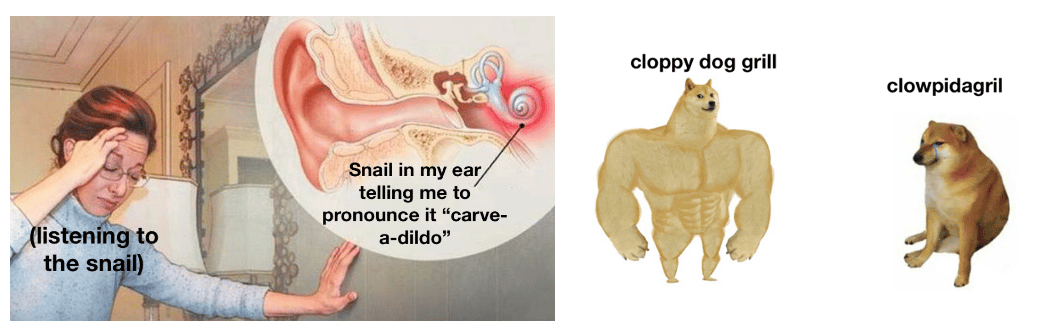
“Err … cloppy-dog-grill?”
Classic. We’ve all butchered a drug name and felt our clinical cred collapse quicker than a 90 year old’s veins.
Sadly, juniors everywhere suffer from mispronouncitis: a tragic condition characterised by vowel invention and incoherent mumbling when put on the spot.
Leading reports even suggest as many as five medical students per day ask an elderly gentleman if he’s taking his ‘fine-ass-to-ride’ for his BPH
Mispronuncitis has a list of triggers longer than acute pancreatitis. But it's undoubtedly most endemic within those prescribing Monoclonal antibodies – as they’re all just names of IKEA furniture, with -amab slapped onto the end.
Take inebilizumab for example:
Unpronounceable? ✅
Sounds like a hex from Harry Potter? ✅
Worth paying attention to? Definitely, if you want to ✨dazzle✨ the neuro consultants and atone for your pronunciation sins.
But how does it even work?
In-a-billy-zoo-mab targets autoimmune CD19+ B cells. It prevents them attacking the NMJ thus preventing worsening autoimmune myasthenia gravis.
Targeting CD19 rather than its famous cousin CD20 means it catches B cells earlier in their development, something not explored before.
Cue the MINT trial, conducted by researchers published in the New England Journal of Medicine.
This was a phase 3, double-blind RCT investigating inebilizumab vs placebo for patients with generalised myasthenia gravis. They recruited 238 participants who were either:
Positive for anti-acetylcholine-receptor (AChR) antibodies OR
Anti-muscle-specific tyrosine kinase (MuSK) antibodies.
All participants got doses of inebilizumab (300mg on day 1 and day 15) or placebo. MuSK-positive patients were followed to 26 weeks, (AChR)-positive participants were to 52 weeks
The main outcome was the change in the MG-ADL* score (+ the QMG† score) at week 26 - i.e. did patients’ day-to-day muscle fatigue and weakness improve?
And what did they find
By week 26 the mean change in MG-ADL was -4.2 with inebilizumab vs -2.2 with placebo (adjusted difference -1.9, 95% CI -2.9 to -1.0; P<0.001)
QMG results also scored in favour of the mab: -4.8 vs -2.3 (adjusted difference -2.5, P<0.001
And despite headaches, coughs and UTIs all noted as side effects, there was no clear increase in serious adverse events compared to placebo.
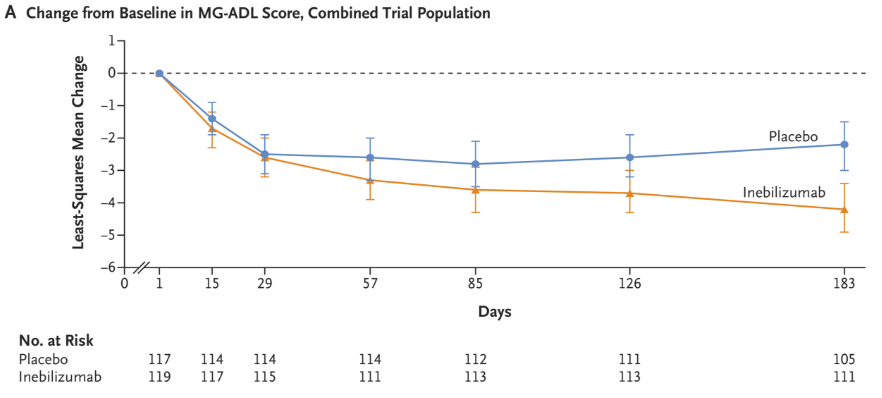
So at least compared to no treatment, Inebilizumab is pretty convincing 👍
Some caveats: not a huge sample size, long-term safety still TBD and monoclonals come with a price tag that makes Zone 2 London rent look affordable.
Plus not every MG patient is AChR/MuSK positive (shoutout to the unlucky seronegatives👋).
That’s said inebilizumab looks to have a bright future…
Effective, well tolerated, and guaranteed to join the “Drugs I Can’t Pronounce” Hall of Fame, right next to clopidogrel and leve .. leve tira … leve-tira-see-ta.. nah, forget it.
*Myasthenia Gravis Activities of Daily Living scale. Higher score = more disease activity
†Quantitative Myasthenia Gravis scale. Again, higher score = more points to myasthenia
QUICKBITS: OTHER NEWS YOU SHOULD KNOW
Competition Ratios are F****ed - A full write up on this is coming next week, but the headline says it all really. The pressure is getting worser. Psych training = 22:1, Obs&Gyn = 17:1, Emergency Med = 14:1, Cardiothoracic Surgery 😂 😂 😂…. 74:1. Have a look yourself using the link above. Like I said, full write up next week.
Exception Reporting Gets an Upgrade – The BMA secured big changes to how we log extra hours. No more waiting weeks or begging supervisors. You’ll get 28 days to submit, 7–10 days for payment/TOIL, and a real choice between the two. Missed deadlines = fines for trusts. Sign-off moves from supervisors to HR/Guardians, with confidentiality protections baked in. Full roll-out by Feb 2026.
RCPsych back Ketamine for Depression - Last week we wrote about MDMA in trials, now RCPsych are backing this psyedelic in practice. Cool. With some caveats of course. It much be used in a “controlled clinical setting”, this is not the go ahead for self-perscription. It’s still interesting to see taboo drugs rebranded as clinically useful.
Multiparametric vs Biparametric MRI’s for Prostate Cancer - So I know if I asked you, “whats the investigation for prostate cancer?” You’d blurt out “multiparatric MRI 🤓”, but what even is a multiparatric MRI? I don’t know, but what I do know is that a biparamtric MRI is now non-inferior according to this trial. That’s a big win for the biparametric community.
Handover Over 🫡
If you liked it, tell your mates**.
If you hated it, tell your enemies.
This poll is upgraded… now when you vote you can give feeback too. Let’s hear your thoughts and vote in the pole below 👇
What did you think about todays handover?
**Final Week of The Handover FIGs Scrub giveaway
7 days left of the challenge.
The top referrer for the Handover at the end of September will get a free pair of FIGs scrubs. Although, I think our frontrunner has run away with it… 100 verified emails is what Ella has got. My goodness.
There isn’t much hope in beating that, but thats alright.
At the last minute we’ve thrown bonus prizes for 2nd and 3rd place.
A Free Pair Crocs Surgical Clogs in your size!
And to break top 3? 14 referrals is the number to beat.
Think you can do it?
Give it a shot and share using your personal referral link below.
N.B. Referral gotta be nhs.net, doctors.net or university email address.
Referral requires double opt in verification, so tell your mates to check their email after they sign up!
Good luck!
Humour me. I was having an discussion about AI Scribe Apps in the clinical settting. Are you partial to any? Which ones have you used? Thank you!
Which have you tried?
Fun Fact: The reason epinephrine/adrenaline has two names is because epi-nephros is Greek for “on kidney”, and ad-renal is the Latin for “on kidney”.
If you want to get in contact with The Handover, email us at [email protected]