
👋 Happy Friday. So who’s gunna win? 100 guys or a gorilla. My money’s on 100 guys, unless the gorilla reads our medical news every week. In which case, it gets really smart and we’re gunna have a whole Planet of the Apes situation go down.
Here are the stories:
🩺 Breaking Clot: The Grey Area in VTE Management
💊 Methotrexate Murder Mystery: It Was The Kidney All Along
🩸 Antiplatelet Wars: Clopidogrel Strikes Back
🧒 The Childhood Vaccine Schedule Update
#TheMoreYouKnow: Other Top Stories of The Week
NHS NEWS
🩺 UKMLA Passed! Time to Supervise Your Own PA(Somehow?)
Congrats to all the students passing the UKMLA and are soon new doctors! Once again, you’ll be starting as the infants of the medical profession. I know it’s daunting starting work, but let’s go through the list of responsibilities to get you prepared for ward monkey duties in August:
Cannulating patients with ‘great veins’✔️
Translating consultants mumble into full SOAP notes✔️
Supervising PA’s ✔️… wait supervising PA?
So the GMC dropped a document outlining some ‘good practice advice’ for the supervision of physician and anesthesia associates. This document has caused a bit of hysteria from the RCP, BMA and DOX –Doctors of X(I just made that up, but it’s got a ring to it).
The GMC’s document explains the principles in which doctors and associates could work together and co-exist like ebony and ivory. Kinda. It mainly states what PA’s/AA’s can and cannot do, and who supervises them. The latter point makes for a bit of grey area.
The GMC guidance states the supervising ‘role will usually be taken by a consultant, GP or autonomously practicing SAS doctor’. Problem being, they didn’t explicitly state juniors couldn’t be held responsible. Let’s take a situation where it’s just a FY1/Y2 on the ward. Since, ‘PA’s and AA’s can’t work completely independently of supervision’ if they misdiagnose a patient, the accountability could fall on the resident.
The BMA started by criticising the whole document, calling it an “unhelpful contribution”.
The RCP followed by saying the new guidance is “disappointing”.
They both agreed that only senior doctors(consultants, GP’s and SAS doctors) should be accountable.
Ultimately, it’s just guidance. A helpful nudge in the right direction haha 🙃. The RCP also published their own interim guidance last December. This one explicitly says it should only be the seniors in charge. Dr Hilary Williams(RCP clinical vice president) urges trusts and boards to follow RCP guidance.
If nothing else, here's a word to the wise: when your PA says, “Don’t worry, I’ll handle it,” that could be your cue to worry.
RESEARCH UPDATE
✂️ Snip Smarter: No-Touch Vein Harvesting Saves CABG’s
Hey, Hey, Hey. Don’t be rough! You’ve got to be delectate, be gentle. You can’t just manhandle the graft. It’s probably the patient's first time. Be considerate. Take it easy. In fact, it might be better if you didn’t touch it at all…
Coronary artery bypass grafting(CABG) isn't new. When you can’t balloon and stent the occluded vessel, you have to replace it. Arterial grafts may be preferred, but 80% of all grafts used are saphenous vein grafts(SVG’s).
Therein lies our problem… SVG’s love to fail.
10-15% fail after one year and that number increases with time. This results in adverse outcomes like angina, MI’s and death. All that surgical effort just to get blocked again in 12 months. Why might that be?
The PATENCY trial, conducted in China and published in the BMJ, thinks it might have something to do with the vein harvesting technique.
Traditionally, we strip off the vein’s outer layer(adventitia) and inflate the vein like a bike tire. The “no-touch” technique skips the abuse. It leaves the vein's outer structure and surrounding tissue intact, theoretically preserving the endothelium and reducing inflammation. Thus reducing occlusion risk
So in theory, it checks out. So they tested it.
A multi-centre RCT with over 2,600 patients, tracking outcomes for three years after surgery. The big question: does this technique actually keep veins open longer?
Who came out on top?
Vein graft occlusion at year 3: No touch: 5.7%. Traditional: 9.0%.
Non-fatal MI’s: No touch: 1.1%. Traditional: 2.2%.
Repeat revascularization: No touch: 6.2%. Traditional: 8.4%.
Readmission for cardiac arrest: No touch: 7.1%. Traditional: 10.2%
So regarding the heart itself. We have a clear winner. However, let's not forget about the leg we took the thing from.
Leg wound complications requiring surgical intervention were significantly higher than in the traditional group(10.3% vs 4.3%, odds ratio: 2.55).
Not cute.
Ultimately, your heart might be grateful, but your leg might file a complaint. Still, if keeping the graft open means one less trip to the cath lab? It might be worth the limp.
Here’s a really nice visual abstract from the BMJ.
MEDTECH/NHS UPDATE
📸 DERM meets Derm: AI Dermatology App for NHS
Is it rude to use your phone in a consultation with a patient? Not when it comes to dermatology.
Is it rude to ask an AI for help to diagnose a condition? Not when it comes to dermatology.
“Doc, is it serious?”
“One second, let me ask Siri real quick”
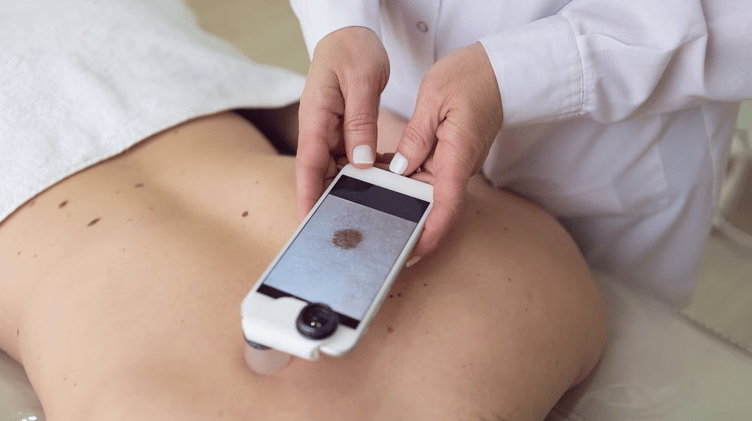
DERM, short for Deep Ensemble for Recognition of Malignancy, is an AI as a Medical Device (AIaMD) developed by Skin Analytics. Unlike many AI tools that serve as decision support, DERM has achieved UKCA Class IIa certification, allowing it to autonomously assess skin lesions and make referral decisions without a doctor's oversight.
This AI is supported by a mobile app, and a special lens that encompasses the skin lesion. And it's just been approved for use in the NHS.
How does it work? DERM uses an algorithm to analyse an image of the skin lesion, then compares it to its knowledge base of skin conditions it’s been trained on.
The aim is to optimise triage of suspicious lesions, hopeful reducing the one million referral each year for dermatology services.
If the app identifies the lesion as precancerous or cancerous, a NHS dermatologist gets called to review it virtually and make a plan. If DERM determines it as benign, the patient is discharged from the urgent pathway and gets results via telephone or letter a little bit later. Handy, if routed in rigorous evidence.
And rigorous it is. In the DERM-003 study, the AI was tested using dermoscopic images from three smartphones, and delivered consistently high diagnostic accuracy:
iPhone 6S: AUROC of 0.88 (SCC), 0.87 (BCC)
iPhone 11: AUROC of 0.88 (SCC), 0.89 (BCC)
Samsung S10: AUROC of 0.85 (SCC), 0.87 (BCC)
It generated results on par with dermatologists, with a phone older than a year 7 student.
Much like the technologies of the last couple weeks, this device has a probation period. It will be trialled over the next three years while further evidence is collected. Once published, NICE will reevaluate and decide if it's worth it.
RESEARCH UPDATE
✌️Peace-out PSA: Saliva Sample For Prostate Cancer Screening
Let’s be honest. It's pretty well-known that the PSA test is a pretty ass screening tool.
I mean, with its false negatives(around 15%), poor sensitivity, and levels rising from a particularly vigorous Peloton session… remind me why we use this thing again?
Because we haven’t really got much else. I mean besides an MRI, a huge and expensive step-up investigation, we really have got to cross our fingers and guess… sorry, use our clinical judgement.
But a new study in The New England Journal of Medicine says we could be onto something better. The BARCODE1 trial took thousands of men, spat in a tube, crunched some DNA data to create a polygenic risk score(PRS).
This score uses genome-wide association studies to look for single-nucleotide polymorphisms(SNPs) associated with a particular disease. In this study, 130 variants were found to create a PRS score for prostate cancer.
The study then aimed to put PRS to the test and see if it could improve detection of clinically significant disease compared to conventional approaches(e.g. PSA based-screening).
What did they do? Researchers invited over 40,000 men, 55-69 in the UK to participate. 6,393 ended up having their PRS calculated from their saliva. Men with a PRS in the top 10% were offered further investigations(PSA test, MRI and a biopsy) and a cancer diagnosis was determined.
So what did they find…
Of those screened 745(11%) had PRS in the 90th percentile and were invited for further tests. 468(62.8%) of those ended up going.
Prostate cancer was diagnosed in 40% of those tested (187/468).
55%(103) had intermediate-high risk. 21.4%(40) had high-very high risk disease.
And the most interesting part of it all. Of the 103 intermediate-high risk individuals diagnosed, 71.8%(74) would not have been detected by the UK’s current pathway. The positive predictive value showed the proportion of clinically significant cancers detected was higher than PSA or MRI alone.
No study is not without its limitations. This study only used men of European ancestry. What happened to DEI 😓? Only 22% of invited men expressed interest, so not all high-risk individuals were screened. And it’s still an ongoing study– long-term outcomes like mortality reduction and overdiagnosis rates aren’t available yet
Bottom line: PSA you’ve had you run? But maybe there is a new screening test on the block.
OTHER NEWS YOU SHOULD KNOW
Handover Over 🫡
If you liked it, tell your mates.
If you hated it, tell your enemies.
Once again, so many new faces! Welcome to the Handover. Let me know what you thought in the poll below!
What did you think about todays handover?
If you’d like to be involved with The Handover, interviewing clinicians in your dream roles, or writing articles on the latest happenings in the world of Medicine, reply to this email